History
CC:
“I feel weak and didn’t eat” x 3 days.
HPI:
Pt is a 35 year old male with PMHx of diabetes mellitus type 1, alcohol abuse and gastritis who presents to the ED complaining of weakness, loss of appetite and diarrhea x3 days. Pt had 3-4 episodes of diarrhea over the past 3 days. Pt also admits to having a non-productive cough, feeling chills and sleeping a lot more than usual x5 days. Pt admits to drinking 2 pints of tequila daily, with his last drink being yesterday. Pt also mentions that he has 10/10 pain down the midline of his abdomen. The pain is described as a burning pain that got really bad after he drank tequila. Pain does not radiate and has been constant x2 days, worse after drinking alcohol. Pt has experienced similar pain and got medication (unknown) from the hospital which are not working recently. Change in position does not exacerbate or relieve the pain. This morning patient experienced 2 episodes of non-bloody, non-bilious vomiting. Pt admits to feeling anxious, feeling pins and needles on his skin and being sensitive to light since this morning. Pt also admits to urinary frequency. Pt was hospitalized for complications of diabetes (though he was unsure what his dx was) 4 months ago and admits to feeling similar to how he feels now. Pt says he is compliant with his insulin, but admits that the last time he took it was 2 nights ago.
Denies headache, shortness of breath, dizziness, hemoptysis, palpitations, hematuria, dysuria, seizures, auditory/visual/tactile hallucinations, dry skin, muscle aches.
PMHx:
- Diabetes mellitus type 1 x unknown years, unknown if controlled as pt mentions last time he took insulin 2 days ago (unknown compliance)
- Hospitalized 4 months ago for unknown complication
- Alcohol abuse x unknown years
- Gastritis x unknown years
Medications:
- Insulin, unknown specific type and dose
- Omeprazole 40 mg QD-TID
- Denies herbal supplement use.
Surgical History:
- No past surgical history.
Allergies:
- No known drug/food/environmental allergies
Family History:
- Unknown
- No known family hx of HTN, cancer. Mom and sister both with type 1 diabetes mellitus.
Social History:
- Smoking: Denies
- Alcohol: 2 pints of tequila daily with the last drink being yesterday.
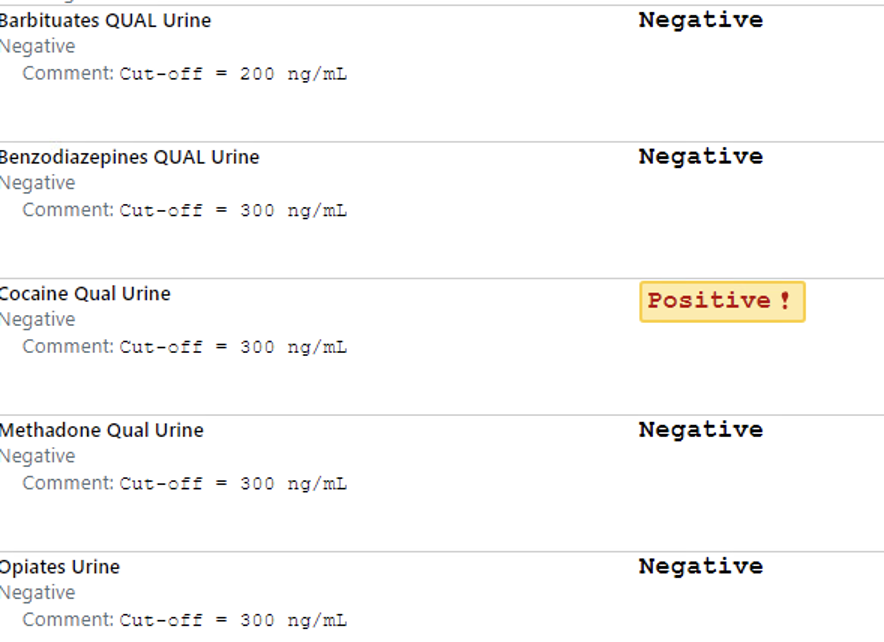
- Illicit drug use: Admits to ocassional use of marijuana, denies past or current use of all other substances.
- Marital History: Single
- Language: Spanish
- Occupational History: Works in a restaurant
- Travel: No recent travel
- Home situation: Lives in homeless shelter
- Sleep: Endorses sleeping more than usual and feeling fatigued.
- Exercise: None
- Diet: Reports loss of appetite x5 days and not really eating much.
- Caffeine: Denies
ROS:
- General: Admits to fever, fatigue, chills and change in appetite. Denies night sweats, weight loss/gain.
- Skin, hair, nails: Denies discolorations, moles, rashes, changes in hair distribution or texture, pruritus.
- HEENT: Denies head trauma, vertigo, visual disturbances, ear pain, hearing loss, tinnitus, epistaxis, discharge, congestion, sore throat, bleeding gums.
- Neck: Denies localized swelling/lumps, stiffness/decreased ROM
- Breast: Denies lumps, nipple discharge, or pain.
- Pulmonary: Admits to cough. Denies dyspnea, wheezing, cyanosis, hemoptysis.
- Cardiovascular: Denies chest pain, edema/swelling of ankles or feet, palpitations.
- Gastrointestinal: Admits to abdominal pain, nausea, vomiting and diarrhea. Denies constipation, dysphagia, pyrosis, flatulence, eructation, rectal bleeding, hemorrhoids or blood in stool.
- Genitourinary: Admits to urinary frequency. Denies nocturia, dysuria, urgency, flank pain, oliguria, polyuria and incontinence.
- Musculoskeletal: Denies joint pain, joint swelling, back pain, muscle pain and arthritis.
- Nervous system: Admits to feeling pins and needles on skin. Denies seizures, headache, loss of consciousness, ataxia, loss of strength, change in cognition/mental status/memory.
- Peripheral vascular: Denies intermittent claudication, coldness or trophic changes, varicose veins, peripheral edema, or color changes.
- Hematologic: Denies anemia, easy bruising or bleeding, lymph node enlargement, history of DVT/PE.
- Endocrine: Admits to diaphoresis. Denies polyuria, polydipsia, polyphagia, heat or cold intolerance, goiter or hirsutism.
- Psychiatric: Denies feelings of helplessness, hopelessness, lack of interest in usual activities, or suicidal ideations, anxiety, obsessive/compulsive disorder, auditory/visual/tactile hallucinations or ever seeing a mental health professional.
Physical
General:
- Well developed, well-nourished, male in mild apparent discomfort appears stated age of 35. Neatly groomed, alert and oriented x3. Dressed appropriately for the weather. Ambulates well without support. Pt appears tremulous at rest, diaphoretic and pale.
Vital Signs:
- BP: 126/68 mm Hg
- R: 19/min, regular rate and rhythm, unlabored
- P: 105 beats per minute, tachycardic, rhythm and amplitude
- T: 100.6 degrees F (oral)
- O2 Sat : 99% room air
- Height: 70 inches Weight: 160 lbs BMI: 23
Skin & Head:
- Skin: Hot and diaphoretic, good turgor. Nonicteric, no lesions, scars, or tattoos noted.
- Nails: No clubbing, cyanosis, or lesions. Capillary refill < 2 seconds in upper and lower extremities.
- Eyes:Symmetrical OU. No strabismus, exophthalmos, or ptosis. Sclera white, cornea clear, conjunctiva pink. PERRLA. EOMs intact with no nystagmus.
Mouth/Pharynx:
- Teeth: Good dentition. No obvious dental caries noted.
- Tongue: Pink and well papillated. No masses, lesions or deviation. Mild fasciculation on exam.
- Oropharynx: Well hydrated. No injection, exudate, masses, lesions or foreign bodies. Tonsils present with no injection or exudate. Grade 1 tonsils. Uvula midline, pink with no edema or lesions.
Thorax and Lungs:
- Chest: Symmetrical, no deformities, no trauma. Respirations unlabored/ no paradoxical respirations or use of accessory muscles noted. Non-tender to palpation throughout.
- Lungs: Clear to auscultation and percussion bilaterally. No adventitious sounds.
Cardiac Exam:
- Heart: Slightly tachycardic with regular rhythm. S1 and S2 are distinct with no murmurs, S3 or S4. No splitting of S2 or friction rubs appreciated.
Abdominal Exam:
- Abdomen flat and symmetric with no scars, striae or pulsations noted. Bowel sounds normoactive in all 4 quadrants with no aortic/renal/iliac or femoral bruits. Tender to palpation in epigastric region and tympanic throughout, no guarding or rebound noted. No hepatosplenomegaly to palpation.
Mental status exam:
- Patient is well appearing, has good hygiene and is neatly groomed. Patient is alert and oriented to name, date, time and location. Speech and language ability intact, with normal quantity, fluency, and articulation. Patient denies changes to mood. Conversation progresses logically. Insight, judgment, cognition, memory and attention intact.
Neurologic Exam:
- Sensation: Sensation is intact bilaterally to pain and light touch. Two-point discrimination is intact.
- Motor:Good muscle tone. Strength is 5/5 bilaterally at the quadriceps, hamstrings, calves and ankles. Tremor present throughout the body at rest.
Differential diagnosis:
- Alcohol withdrawal syndrome (AWS)
- Alcohol withdrawal syndrome is characterized by tachycardia, tremors, diaphoresis and anxiety initially. AWS can develop into delirium tremens and quickly become fatal. Therefore, it is important to identify this diagnosis early and begin treatment as soon as possible. Given that this patient was experiencing those symptoms and that he is a heavy alcohol drinker who recently stopped drinking, this makes AWS very likely in this patient. We used the Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) tool to assess for AWS. It is a tool used to assess whether AWS is present. Pts who score below 8 do not require treatment. Between scores 8-10 treatment should be initiated and a score over 20 may require ICU admission. This pt initially had a CIWA score of 15.
- Diabetic ketoacidosis
- This pt has a history of type 1 diabetes and admits to not taking his insulin for the past 2 days. This pt also presents with many of the symptoms of DKA including nausea, vomiting, abdominal pain, weakness and fever.
- Gastritis
- This pt has previously been diagnosed with gastritis. He admits that the medications he was taking was helping, however recently not as much. This diagnosis is likely in this pt because the pain was described as a sharp pain in the midline (epigastric region) and was worsened with the drinking of alcohol, characteristic of gastritis.
- Acute pancreatitis
- Pancreatitis has abdominal pain, nausea, vomiting, fever and diarrhea. It also may cause respiratory symptoms if the pancreas becomes inflamed and irritates the diaphragm. These are all symptoms that the pt is experiencing. Additionally, a very common cause of pancreatitis is alcohol consumption. Additionally, the pain in pancreatitis is said to be constant, as this pt is experiencing. However, this diagnosis is not as likely being that he described the pain as sharp, whereas in pancreatitis it is usually a gnawing pain. Also position changes did not help with the pain as expected in pancreatitis.
- Viral respiratory infection (covid/flu/RSV)
- This pt has been experiencing a dry cough, fever and weakness for 5 days, even before he had his last alcoholic drink. Also, he lives in a shelter and these viral illnesses are going around at this time of year. This cannot be excluded without testing. Being that he is at high risk for complications due to his AWS testing should be done, so treatment could be initiated.
Labs:
- POC glucose
- 135 mg/dL (reference: 70-110 mg/dL)
- Lipase
- 73 U/L (reference: 13-60 U/L)
- Magnesium
- 1.3 mg/dL (reference: 1.4-2.6 mg/dL)
- Covid/Flu A and B swab
- Flu A positive
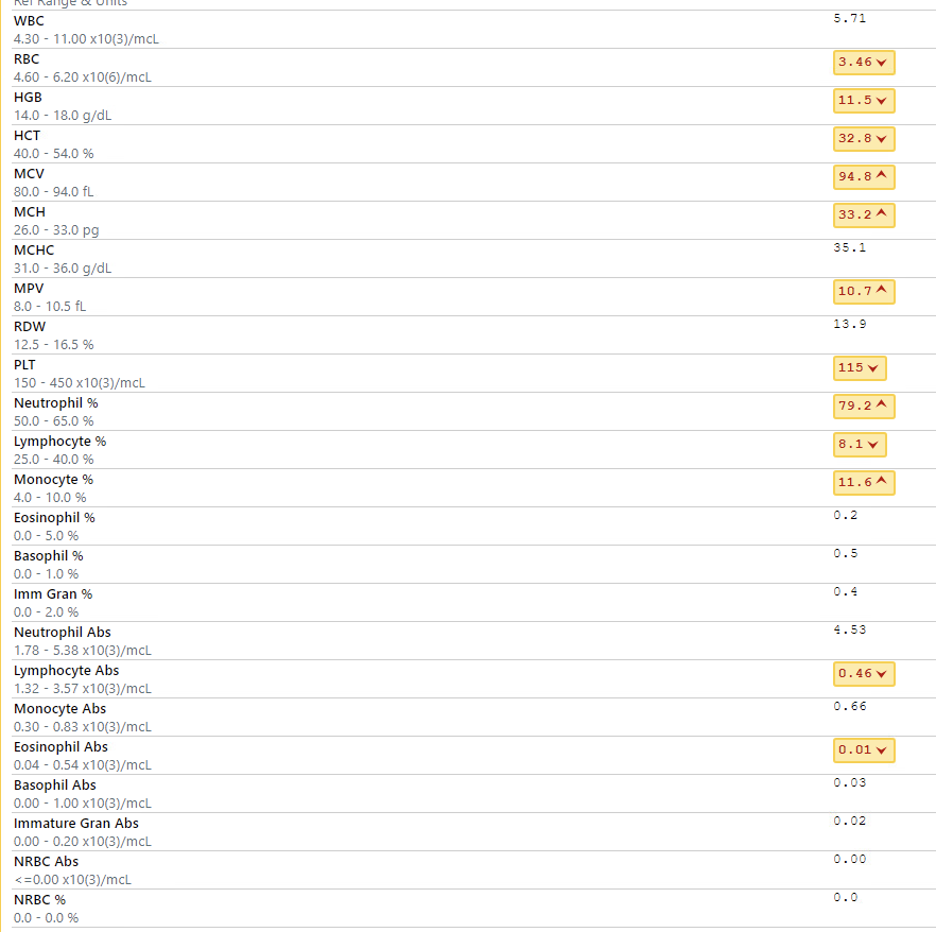
- CBC with diff.
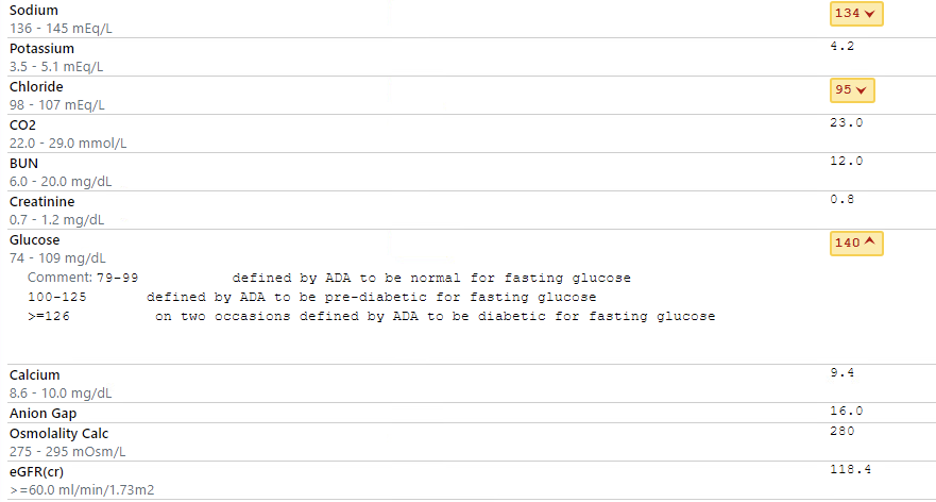
- BMP
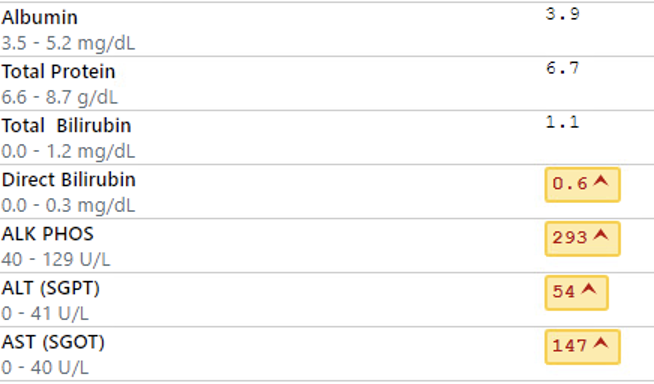
- Hepatic function panel
- Drug screen
Assessment
- 35 year old male with PMHx of type 1 diabetes mellitus, gastritis and alcohol abuse presents complaining of cough, fatigue and weakness x3-5 days. Pt also experienced 2 episodes of vomiting this morning and is complaining of severe pain in the midline of his abdomen. Pts last alcoholic drink was yesterday, after normally drinking 2 pints of tequila daily. Pt has CIWA score of 15. Vitals are significant for fever and mild tachycardia. On exam pt appears tremulous, pale and diaphoretic. Pt is also tender in the epigastric region, with no rebound or guarding. All other parts of the exam are within normal limits. Labs are significant for macrocytic anemia and elevated liver enzymes, likely due to his history of alcohol abuse. Pt also tested positive for flu A. All other labs are not significantly high or low. At this time, based on the labs and physical exam, there is concern for alcohol withdrawal syndrome and gastritis flare up.
Diagnosis:
- Alcohol withdrawal syndrome
- Flu A
- Gastritis
Plan
- Supportive care
- Ondansetron 4 mg IV once
- 1,000 mL normal saline
- Acetaminophen 1,000 mg PO Q4-6H PRN pain
- Flu A
- Droplet isolation
- Oseltamivir 75 mg BID x5 days
- Alcohol withdrawal syndrome
- Chlordiazepoxide 50 mg PO once
- Diazepam 5 mg IV push once
- Lorazepam 2 mg IV
- Gastritis
- Famotidine 20 mg IV push once
- Diabetes
- Recheck blood glucose Q2H
- Initiate insulin regimen
- Internal medicine consult for admission

